Search
- Page Path
- HOME > Search
- Thyroid
Big Data Articles (National Health Insurance Service Database) - Risk of Diabetes in Patients with Long-Standing Graves’ Disease: A Longitudinal Study
- Eyun Song, Min Ji Koo, Eunjin Noh, Soon Young Hwang, Min Jeong Park, Jung A Kim, Eun Roh, Kyung Mook Choi, Sei Hyun Baik, Geum Joon Cho, Hye Jin Yoo
- Endocrinol Metab. 2021;36(6):1277-1286. Published online December 16, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1251
- 5,179 View
- 181 Download
- 9 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
The detrimental effects of excessive thyroid hormone on glucose metabolism have been widely investigated. However, the risk of diabetes in patients with long-standing hyperthyroidism, especially according to treatment modality, remains uncertain, with few longitudinal studies.
Methods
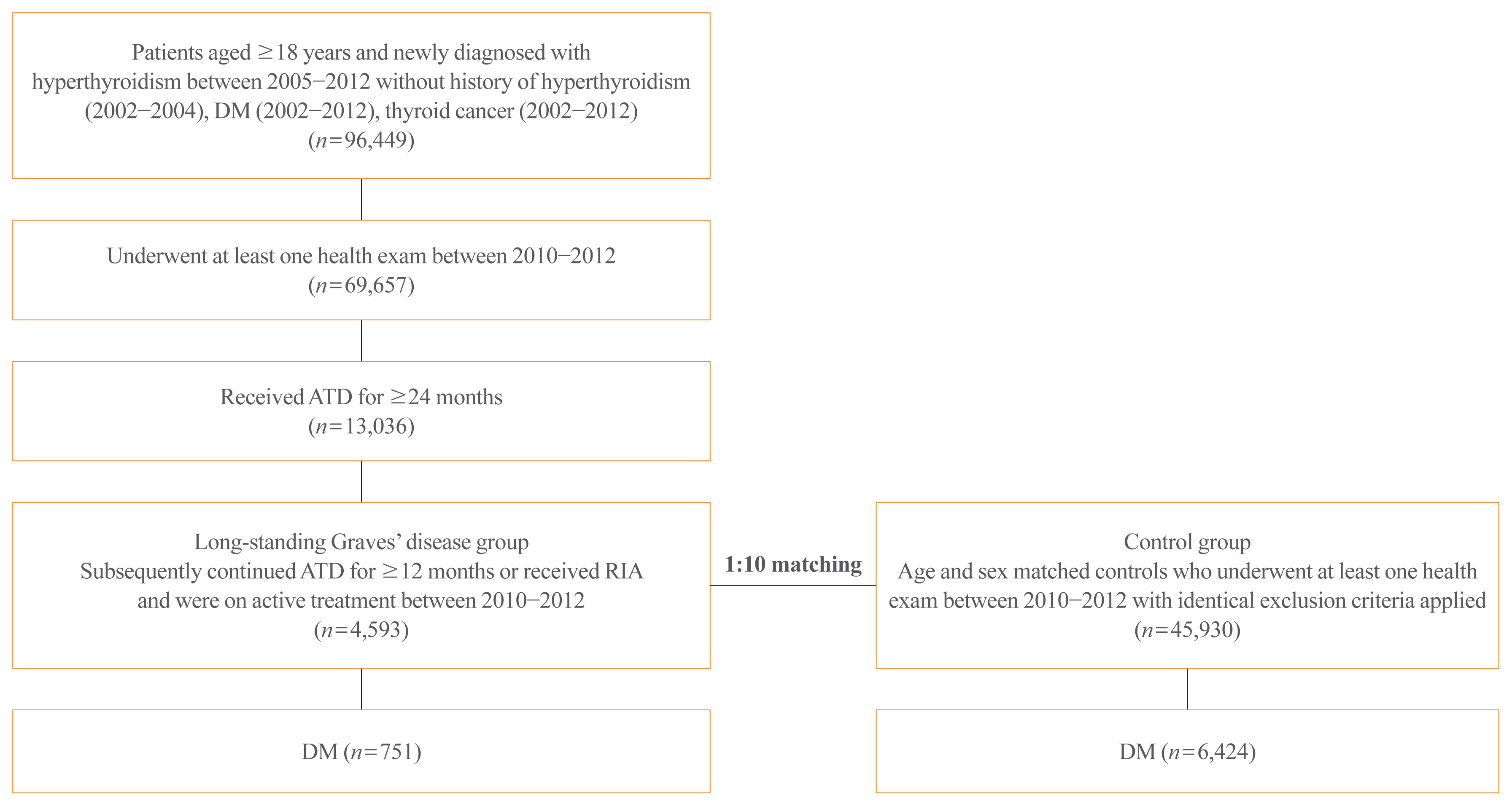
The risk of diabetes in patients with Graves’ disease treated with antithyroid drugs (ATDs) for longer than the conventional duration (≥2 years) was compared with that in age-and sex-matched controls. The risk was further compared according to subsequent treatment modalities after a 24-month course of ATD: continuation of ATD (ATD group) vs. radioactive iodine ablation (RIA) group.
Results
A total of 4,593 patients were included. Diabetes was diagnosed in 751 (16.3%) patients over a follow-up of 7.3 years. The hazard ratio (HR) for diabetes, after adjusting for various known risk factors, was 1.18 (95% confidence interval [CI], 1.10 to 1.28) in patients with hyperthyroidism. Among the treatment modality groups, the RIA group (n=102) had a higher risk of diabetes than the ATD group (n=4,491) with HR of 1.56 (95% CI, 1.01 to 2.42). Further, the risk of diabetes increased with an increase in the ATD treatment duration (P for trend=0.019).
Conclusion
The risk of diabetes was significantly higher in patients with long-standing Graves’ disease than in the general population, especially in patients who underwent RIA and prolonged ATD treatment. Special attention to hyperglycemia during follow-up along with effective control of hyperthyroidism may be necessary to reduce the risk of diabetes in these patients. -
Citations
Citations to this article as recorded by- Safety of non-standard regimen of systemic steroid therapy in patients with Graves’ orbitopathy: a single-centre experience
Nadia Sawicka-Gutaj, Dawid Gruszczyński, Natalia Zawalna, Kacper Nijakowski, Agnieszka Skiba, Mateusz Pochylski, Jerzy Sowiński, Marek Ruchała
Pharmacological Reports.2024; 76(1): 185. CrossRef - Increased risk of diabetes mellitus and hyperlipidemia in patients with differentiated thyroid cancer
Hwa Young Ahn, Jooyoung Lee, Jinmo Kang, Eun Kyung Lee
European Journal of Endocrinology.2024; 190(3): 248. CrossRef - Prevalencia de diabetes en personas con disfunción tiroidea
Juan J. Díez, Pedro Iglesias
Medicina Clínica.2023; 160(8): 333. CrossRef - Control of Thyroid Dysfunction in Spanish Population Registered in
the Primary Care Clinical Database: An Analysis of the Proportion of Patients
with Thyrotropin Values Outside the Reference Range
Juan J. Díez, Pedro Iglesias
Hormone and Metabolic Research.2023; 55(03): 184. CrossRef - Prevalence of thyroid dysfunction and its relationship to income level and employment status: a nationwide population-based study in Spain
Juan J. Díez, Pedro Iglesias
Hormones.2023; 22(2): 243. CrossRef - Prevalence of diabetes in people with thyroid dysfunction
Juan J. Díez, Pedro Iglesias
Medicina Clínica (English Edition).2023; 160(8): 333. CrossRef - Diabetes Mellitus Secondary to Endocrine Diseases: An Update of Diagnostic and Treatment Particularities
Mihaela Simona Popoviciu, Lorena Paduraru, Raluca Marinela Nutas, Alexandra Maria Ujoc, Galal Yahya, Kamel Metwally, Simona Cavalu
International Journal of Molecular Sciences.2023; 24(16): 12676. CrossRef - Thyroid Eye Disease and Its Association With Diabetes Mellitus: A Major Review
Roshmi Gupta, Pramila Kalra, Lakshmi B. Ramamurthy, Suryasnata Rath
Ophthalmic Plastic & Reconstructive Surgery.2023; 39(6S): S51. CrossRef - Metabolite Changes during the Transition from Hyperthyroidism to Euthyroidism in Patients with Graves’ Disease
Ho Yeop Lee, Byeong Chang Sim, Ha Thi Nga, Ji Sun Moon, Jingwen Tian, Nguyen Thi Linh, Sang Hyeon Ju, Dong Wook Choi, Daiki Setoyama, Hyon-Seung Yi
Endocrinology and Metabolism.2022; 37(6): 891. CrossRef - Diabetes and Hyperthyroidism: Is There a Causal Link?
Sang Yong Kim
Endocrinology and Metabolism.2021; 36(6): 1175. CrossRef
- Safety of non-standard regimen of systemic steroid therapy in patients with Graves’ orbitopathy: a single-centre experience

- Clinical Study
- Impact of the Dynamic Change of Metabolic Health Status on the Incident Type 2 Diabetes: A Nationwide Population-Based Cohort Study
- Jung A Kim, Da Hye Kim, Seon Mee Kim, Yong Gyu Park, Nan Hee Kim, Sei Hyun Baik, Kyung Mook Choi, Kyungdo Han, Hye Jin Yoo
- Endocrinol Metab. 2019;34(4):406-414. Published online December 23, 2019
- DOI: https://doi.org/10.3803/EnM.2019.34.4.406
- 5,985 View
- 84 Download
- 16 Web of Science
- 19 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub Background Metabolically healthy obese (MHO) is regarded as a transient concept. We examined the effect of the dynamic change of metabolic health status on the incidence of type 2 diabetes mellitus (T2DM) both in obese and normal weight individuals.
Methods We analyzed 3,479,514 metabolically healthy subjects aged over 20 years from the Korean National Health Screening Program, who underwent health examination between 2009 and 2010, with a follow-up after 4 years. The relative risk for T2DM incidence until the December 2017 was compared among the four groups: stable metabolically healthy normal weight (MHNW), unstable MHNW, stable MHO, and unstable MHO.
Results During the 4 years, 11.1% of subjects in the MHNW group, and 31.5% in the MHO group converted to a metabolically unhealthy phenotype. In the multivariate adjusted model, the unstable MHO group showed the highest risk of T2DM (hazard ratio [HR], 4.67; 95% confidence interval [CI], 4.58 to 4.77). The unstable MHNW group had a higher risk of T2DM than stable MHO group ([HR, 3.23; 95% CI, 3.16 to 3.30] vs. [HR, 1.81; 95% CI, 1.76 to 1.85]). The stable MHO group showed a higher risk of T2DM than the stable MHNW group. The influence of the transition into a metabolically unhealthy phenotype on T2DM incidence was greater in subjects with aged <65 years, women, and those with weight gain.
Conclusion Metabolically healthy phenotype was transient both in normal weight and obese individuals. Maintaining metabolic health was critical for the prevention of T2DM, irrespective of their baseline body mass index.
-
Citations
Citations to this article as recorded by- Metabolically healthy obese individuals are still at high risk for diabetes: Application of the marginal structural model
Hye Ah Lee, Hyesook Park
Diabetes, Obesity and Metabolism.2024; 26(2): 431. CrossRef - Association of anthropometric parameters as a risk factor for development of diabetic retinopathy in patients with diabetes mellitus
Aditya Verma, Ashok Jha, Ahmed Roshdy Alagorie, Rishi Sharma
Eye.2023; 37(2): 303. CrossRef - From Metabolic Syndrome to Type 2 Diabetes in Youth
Dario Iafusco, Roberto Franceschi, Alice Maguolo, Salvatore Guercio Nuzio, Antonino Crinò, Maurizio Delvecchio, Lorenzo Iughetti, Claudio Maffeis, Valeria Calcaterra, Melania Manco
Children.2023; 10(3): 516. CrossRef - Assessment of Metabolic Syndrome Risk Based on Body Size Phenotype in Korean Adults: Analysis of Community-based Cohort Data
Ji Young Kim, Youngran Yang
Research in Community and Public Health Nursing.2023; 34: 158. CrossRef - Dynamic Changes in Metabolic Status Are Associated With Risk of Ocular Motor Cranial Nerve Palsies
Daye Diana Choi, Kyung-Ah Park, Kyungdo Han, Sei Yeul Oh
Journal of Neuro-Ophthalmology.2023;[Epub] CrossRef - New metabolic health definition might not be a reliable predictor for diabetes in the nonobese Chinese population
Liying Li, Ziqiong Wang, Haiyan Ruan, Muxin Zhang, Linxia Zhou, Xin Wei, Ye Zhu, Jiafu Wei, Xiaoping Chen, Sen He
Diabetes Research and Clinical Practice.2022; 184: 109213. CrossRef - Metabolically healthy obesity: Is it really healthy for type 2 diabetes mellitus?
Qi Wu, Ming-Feng Xia, Xin Gao
World Journal of Diabetes.2022; 13(2): 70. CrossRef - Metabolically obese phenotype and its dynamic change are associated with increased carotid intima-media thickness: Results from a cohort study
Liping Yang, Xue Li, Li Wang, Shan Xu, Yanmei Lou, Fulan Hu
Nutrition, Metabolism and Cardiovascular Diseases.2022; 32(9): 2238. CrossRef - Obesity Metabolic Phenotype, Changes in Time and Risk of Diabetes Mellitus in an Observational Prospective Study on General Population
Chan Yang, Xiaowei Liu, Yuanyuan Dang, Juan Li, Jingyun Jing, Di Tian, Jiangwei Qiu, Jiaxing Zhang, Ni Yan, Xiuying Liu, Yi Zhao, Yuhong Zhang
International Journal of Public Health.2022;[Epub] CrossRef - Implications of metabolic health status and obesity on the risk of kidney cancer: A nationwide population-based cohort study
Yun Kyung Cho, Hwi Seung Kim, Joong-Yeol Park, Woo Je Lee, Ye-Jee Kim, Chang Hee Jung
Frontiers in Endocrinology.2022;[Epub] CrossRef - Metabolic health is a determining factor for incident colorectal cancer in the obese population: A nationwide population‐based cohort study
Yun Kyung Cho, Jiwoo Lee, Hwi Seung Kim, Joong‐Yeol Park, Woo Je Lee, Ye‐Jee Kim, Chang Hee Jung
Cancer Medicine.2021; 10(1): 220. CrossRef - Cumulative Exposure to Metabolic Syndrome Components and the Risk of Dementia: A Nationwide Population-Based Study
Yunjung Cho, Kyungdo Han, Da Hye Kim, Yong-Moon Park, Kun-Ho Yoon, Mee Kyoung Kim, Seung-Hwan Lee
Endocrinology and Metabolism.2021; 36(2): 424. CrossRef - Excessive Intake of High-Fructose Corn Syrup Drinks Induces Impaired Glucose Tolerance
Hidemi Hattori, Yuma Hanai, Yuto Oshima, Hiroaki Kataoka, Nozomu Eto
Biomedicines.2021; 9(5): 541. CrossRef - The risk of Alzheimer’s disease according to dynamic changes in metabolic health and obesity: a nationwide population-based cohort study
Yun Kyung Cho, Jiwoo Lee, Hwi Seung Kim, Joong-Yeol Park, Woo Je Lee, Ye-Jee Kim, Chang Hee Jung
Aging.2021; 13(13): 16974. CrossRef - Metabolically healthy obesity: predictors of transformation to unhealthy phenotype in St Petersburg population (according to the ESSE-RF study)
M. A. Boyarinova, O. P. Rotar, A. M. Erina, N. A. Paskar, A. S. Alieva, E. V. Moguchaia, E. P. Kolesova, A. O. Konradi
"Arterial’naya Gipertenziya" ("Arterial Hypertension").2021; 27(3): 279. CrossRef - Physiological and Lifestyle Traits of Metabolic Dysfunction in the Absence of Obesity
Hanna Bjørk Klitgaard, Jesper Hoffmann Kilbak, Erica Arhnung Nozawa, Ann V. Seidel, Faidon Magkos
Current Diabetes Reports.2020;[Epub] CrossRef - Exploring Therapeutic Targets to Reverse or Prevent the Transition from Metabolically Healthy to Unhealthy Obesity
Tenzin D. Dagpo, Christopher J. Nolan, Viviane Delghingaro-Augusto
Cells.2020; 9(7): 1596. CrossRef - Prepregnancy smoking and the risk of gestational diabetes requiring insulin therapy
Mee Kyoung Kim, Kyungdo Han, Sang Youn You, Hyuk-Sang Kwon, Kun-Ho Yoon, Seung-Hwan Lee
Scientific Reports.2020;[Epub] CrossRef - Obesity with and without type 2 diabetes: are there differences in obesity history, lifestyle factors or concomitant pathology?
E. A. Shestakova, Yu. I. Yashkov, O. Yu. Rebrova, M. V. Kats, M. D. Samsonova, I. I. Dedov
Obesity and metabolism.2020; 17(4): 332. CrossRef
- Metabolically healthy obese individuals are still at high risk for diabetes: Application of the marginal structural model


 KES
KES

 First
First Prev
Prev



